What is sciatica?
Sciatica is a term used to describe pain, numbness, or tingling that follows the path of the sciatic nerve. While it is frequently characterized by a shooting sensation from the lower back down the leg, it is a common condition that impacts up to 40% of people during their lifetime, with severity ranging from mild discomfort to significant functional impairment.
In this post, we’ll break down the anatomy of the sciatic nerve, common symptoms, and the evidence-based pathways for management.
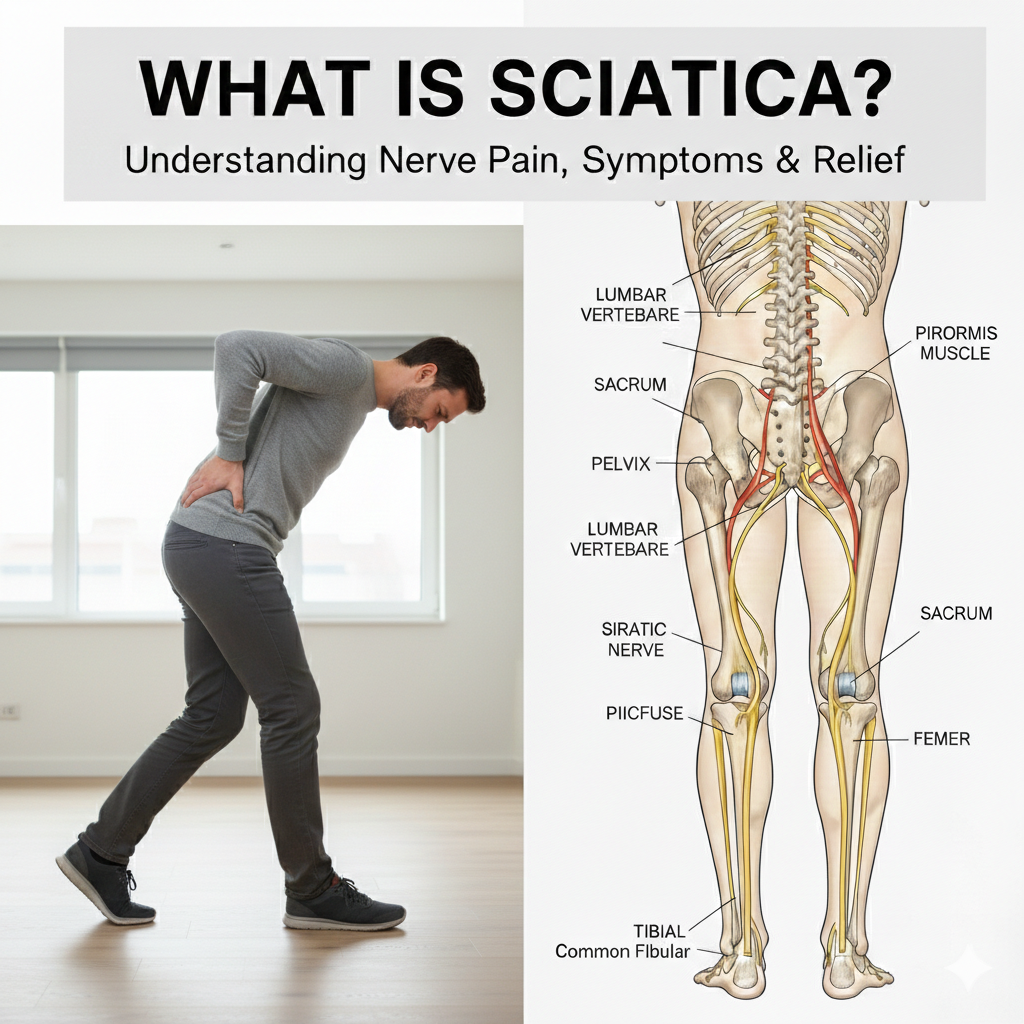
The Anatomy of the Sciatic Nerve
The sciatic nerve is the largest nerve in the human body. It is formed by five nerve roots originating in the lower spine. From there, it runs through the hip and buttock before branching out below the knee to supply the lower leg and foot.
Clinically, a distinction is often made between:
-
True Sciatica: Resulting from direct injury or compression of the sciatic nerve itself.
-
Related Conditions: Symptoms that mimic sciatica but are caused by other spinal or nerve-related issues.
Sciatica is most prevalent in adulthood, particularly after the age of 20, unless a specific physical injury occurs.
Common Symptoms
Sciatica symptoms are often unilateral (occurring on one side of the body) and typically radiate from the lower back or buttock down the leg. Common experiences include:
-
Sensation Type: Sharp, burning, or “electric-like” pain.
-
Physical Triggers: Discomfort that may worsen during coughing, sneezing, bending, or lifting.
-
Neurological Changes: Sensory changes such as tingling (“pins and needles”), numbness, or muscle weakness.
Important Note: Rare but serious symptoms, such as bowel or bladder dysfunction, require urgent medical attention.
Causes and Risk Factors
Sciatica occurs when the nerve roots in the spine are compressed or irritated. Several underlying conditions can lead to this, including:
-
Disc herniation or degenerative disc disease.
-
Spinal or foraminal stenosis.
-
Spondylolisthesis or osteoarthritis.
-
Pregnancy or physical trauma.
Factors That Increase Risk
While a clear cause isn’t always identified, certain factors can increase the likelihood of irritation:
-
Lifestyle: Physical inactivity, prolonged sitting, and poor core strength.
-
Occupational: Physically demanding work or poor lifting mechanics.
-
Health Markers: Aging, excess body weight, diabetes, and tobacco use.
Evidence-Based Treatment Approaches
Current clinical practice guidelines recommend a patient-centered, multimodal approach to managing lower back pain and sciatica. The focus has shifted away from passive bed rest toward active recovery.
1. Education and Self-Management
The foundation of care involves reassuring the individual about recovery expectations and encouraging them to remain active. Supporting a person’s ability to maintain their usual daily activities is a key priority.
2. Multimodal Conservative Care
For most people, a combination of conservative treatments is recommended:
- Structured Exercise: Specific movements to improve function.
- Spinal Manipulation: Often provided through chiropractic care to address movement mechanics.
- Patient Education: Learning how to manage symptoms through movement.
3. Intensive Rehabilitation
For persistent or chronic symptoms, an interdisciplinary approach is often best. This integrates physical exercise with cognitive and behavioral strategies to address the various factors contributing to long-term pain.
4. Medical Management
In the acute stage, medical professionals may consider the short-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) as part of a broader plan, though these are typically not recommended as a stand-alone solution.
Summary
Managing sciatica effectively relies on a focus on function, education, and active care. By following a stepwise approach—starting with conservative, non-invasive options—most individuals can successfully navigate the discomfort and return to their regular lifestyle.
Disclaimer: This content is for educational purposes only and does not constitute medical advice. This information is not intended to replace professional medical advice, diagnosis, or treatment. For individualized advice, always contact your qualified health care provider.
References
-
Cleveland Clinic. (n.d.). Sciatica. https://my.clevelandclinic.org/health/diseases/12792-sciatica
-
Zaina, F., et al. (2023). A Systematic Review of Clinical Practice Guidelines for Persons With Non-specific Low Back Pain With and Without Radiculopathy. Archives of Physical Medicine and Rehabilitation, 104(11), 1913–1927.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.